Physician Value-Based Payment Modifier: What You Need to Know for 2014
The Affordable Care Act (ACA) requires that the Centers for Medicare & Medicaid Services (CMS) apply a value-based modifier (VBM) to Medicare physician fee schedule payments starting with select physicians in 2015 and all physicians by 2017. The VBM will adjust physician payments based on their performance on a composite of quality and cost-of-care measures.
Value-Based Payment Modifier Timeline
- 2012—CMS provided confidential feedback reports to all successful PQRS participants to demonstrate the type of information that will be used to calculate the VBM.
- 2013—Initial performance period began for large group practices only (>100 eligible professionals).
- 2014—Performance period begins for group practices with >10 eligible professionals.
- 2015—(a) Initial application of the payment modifier to large group practices only (>100 eligible professionals) based on 2013 performance. (b) Performance period begins for ALL physicians.
- 2016—Application of the payment modifier to group practices with >10 eligible professionals based on 2014 performance.
- 2017—Application of the payment modifier to ALL physicians based on 2015 performance.
2014 Targeted Populations
Only group practices with 10 or more eligible professionals (EPs) need to take action during the 2014 reporting year to avoid a payment adjustment in 2016 under the VBM. However, solo practitioners and physicians in smaller group practices are encouraged to start participating in the Physician Quality Reporting System (PQRS), which forms the basis of the VBM, since the VBM will be applied to all physicians starting with the 2015 reporting year.
How Is Group Practice Defined?
The size of a group is determined by how many EPs are in the group. A group is defined as a single Tax Identification Number (TIN) with 2 or more individual EPs, identified by Individual National Provider Identifier (NPI), who have reassigned their billing rights to the TIN. For purposes of determining group practice size, EPs are defined as
- Physician
- Physician assistant
- Nurse practitioner or clinical nurse specialist
- Certified registered nurse anesthetist
- Certified nurse-midwife
- Clinical social worker
- Clinical psychologist
- Registered dietitian or nutrition professional
- Physical or occupational therapist or a qualified speech-language pathologist
- Qualified audiologist
Due to this broad definition, smaller practices that rely on ancillary staff could easily fall under the category of 10 or more EPs and will need to take action in 2014 to avoid a 2016 payment adjustment. CMS will identify group practices subject to the 2016 VBM based on a query of Medicare’s Provider Enrollment, Chain, and Ownership System (PECOS) as of October 15, 2014.
Application of the 2016 Value-Based Payment Modifier
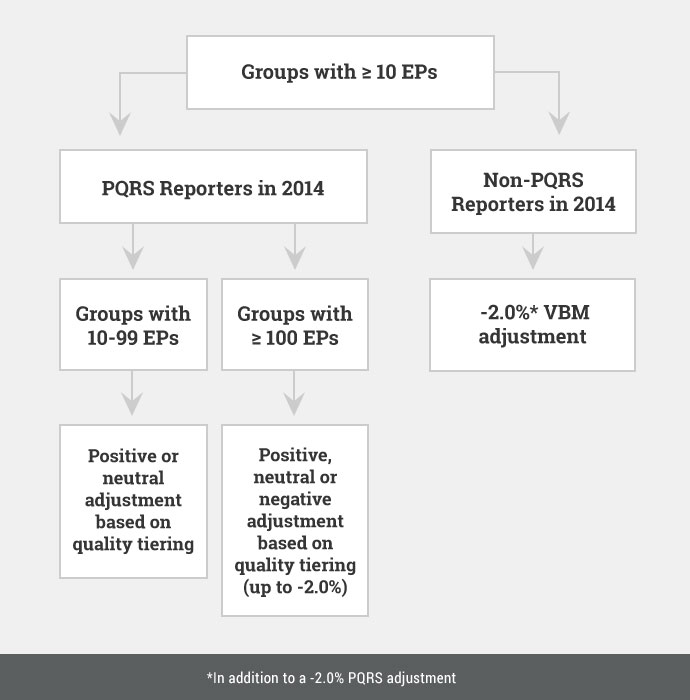
Non-PQRS Reporters in 2014
As illustrated above, group practices with >10 EPs that do not register to participate in the 2014 PQRS as a group (ie, under the Group Practice Reporting Option [GPRO]) and do not satisfy the minimum reporting requirements will receive an automatic -2.0% adjustment to their total annual Medicare paid amounts under the physician fee schedule in 2016. This adjustment is made at the TIN level and applies only to items and services billed by physicians under the TIN, but not other EPs that may comprise the group. The -2.0% VBM adjustment will be applied in addition to the -2.0% adjustment that the group would receive for not satisfying the 2014 PQRS, for a total cut of -4.0%.
NEW FOR 2014. If a group practice does not seek to participate in the PQRS GPRO but at least 50% of EPs in the group satisfy PQRS reporting requirements as individuals, CMS will hold the group harmless from VBM penalties and automatically apply the quality tiering approach described below.
PQRS Reports in 2014
Group practices with >10 EPs that register and successfully participate in the PQRS GPRO in 2014 are held harmless from the automatic VBM cuts (and entitled to a separate 0.5% PQRS incentive payment in 2014). These groups will be subject to “quality tiering,” which is the mechanism by which CMS will evaluate the group’s performance on a composite of quality and cost-of-care measures and use that score to adjust payments. As illustrated above, groups with 10-99 EPs will be held harmless from negative adjustments in 2016 based on 2014 performance.
To calculate the quality composite score, CMS will consider the group’s performance on the following measures:
- Any PQRS measures reported by the group via the selected GPRO reporting method
- Three outcome measures that CMS will automatically calculate based on an analysis of claims
- All-cause readmissions
- Acute preventive quality indicator composite (bacterial pneumonia, UTI, dehydration)
- Chronic preventive quality indicator composite (COPD, HF, DM)
To calculate the cost composite score, CMS will consider performance on the following measures:
- Total per Capita Costs for All Beneficiaries: Evaluates all Medicare Part A and B costs associated with any beneficiary over a year. Beneficiaries are attributed to the group that provided the plurality of primary care services to that individual.
- Total per Capita Costs for Select Conditions: Evaluates a Part A and B costs for patients with specific conditions (HF, CAD, COPD, DM). Beneficiaries are attributed to the group that provided the plurality of primary care services to that individual.
- Medicare Spending per Beneficiary: Evaluates Part A and B costs spanning 3 days prior to and 30 days after an inpatient hospitalization. Beneficiaries are attributed to the group that provided the plurality of Part B services during the inpatient stay.
Since this is a budget-neutral program, spending on upward adjustments for high performers cannot exceed spending on downward adjustments for low performing practices. As shown in the table below, CMS will divide the total quality and cost composite scores for each group practice into three tiers based on whether their score is above, not different from, or below the national mean (with the goal of targeting statistically significant outliers rather than those performing at the mean). Groups that are high quality/low cost will receive the greatest upward adjustment and groups that are low quality/high cost will receive the greatest downward adjustment. After the performance period has ended and the aggregate amount of downward adjustments for 2016 is known, CMS will apply an adjustment factor (“x”) to determine upward payments. To ensure that the VBM does not discourage practices from providing care to more complex or sick patients, CMS also will apply an additional upward payment adjustment for groups treating high-risk beneficiaries.
Calculation of the Value Modifier Using the Quality-Tiering Approach
| Cost/Quality | Low Quality | Average Quality | High Quality |
| Low Cost | +0.0% | +1.0x* | +2.0x* |
| Average Cost | -1.0% | +0.0% | +1.0x* |
| High Cost | -2.0% | -1.0% | +0.0% |
* Groups eligible for an additional +1.0x if average beneficiary risk score is in the top 25% of all beneficiary risk scores
Quality and Resource Use Reports
The Quality and Resource Use Reports (QRURs) are annual reports that CMS provides to group practices with the following information:
- comparative information about the quality and cost of care furnished to their Medicare FFS patients
- beneficiary-specific information to help coordinate and improve the quality and efficiency of care furnished
- information on how the group would fare under the VBM.
In the fall of 2013, 2012 QRURs were made available to all groups of physicians with >25 EPs. A template of the 2012 report can be viewed here. In the late summer of 2014, CMS will distribute 2013 QRURs to all groups and solo practitioners.
It is important to review your QRURs since they will serve as a preview of the VBM methodologies CMS will apply to your practice in the coming years. You are encouraged to use this opportunity to:
- verify the accuracy of EPs billing under your group’s TIN
- determine how your group would fare under the VBM (under “Performance Highlights”)
- examine the number of beneficiaries attributed to your group and the basis for their attribution
- evaluate how your group’s performance on quality and cost measures compares to other groups
- understand which attributed beneficiaries are driving your group’s cost and quality measures
- identify those beneficiaries that are in need of greater care coordination.
CMS has published additional information on how to access your QRUR.
How to Get Started
- Determine your eligibility
Only group practices with >10 EPs have to take action in 2014 to avoid the 2016 VBM penalty (see section “How is Group Practice Defined?” above). However, individuals and groups of all sizes are encouraged to participate in the PQRS in 2014 to avoid a separate PQRS penalty in 2016 and to prepare themselves for 2015 when the VBM applies to ALL physicians. - Register by September 30, 2014
Group practices with >10 EPs must indicate their desire to participate in the PQRS GPRO via the Physician Value-Physician Quality Reporting System (PV-PQRS) Registration System by September 30, 2014. The PV-PQRS requires the use of a valid Individual’s Authorized Access to the CMS Computer Services (IACS) account. During the open registration period, group practices also must specify their GPRO reporting method, though they may change it at any time prior to the September 30, 2014 deadline. Once a group registers for the 2014 PQRS GPRO, it will not be able to withdraw its registration. CMS will analyze claims later in the year to determine which group practices, among those eligible, did not register to participate in the GPRO. CMS will then automatically determine whether at least 50% of individual EPs in those practices satisfied PQRS reporting requirements. These individuals do not have to register with CMS and the group practice does not have to take any action to alert CMS to its individual members’ actions.
You can read more about the VBM and QRURs at the CMS website.
